Head injury in the military

In an excellent article on research being done to address Traumatic Brain Injury (TBI) in the military, The St. Louis Post-Dispatch presents efforts being made to identify the extent of the problem.
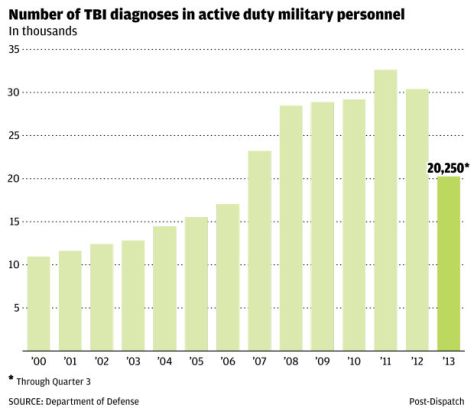
According to researchers there are four kinds of TBI — mild, moderate, severe and penetrating. Since 2000, nearly 300,000 active-duty military personnel have been diagnosed with TBI.
It wasn’t until 2008 that the Department of Defense began to enforce a police of mandatory post-deployment screenings for TBI; and then, in 2010, a mandate for across the board screenings of all personnel exposed to a blast within 50 meters was enforced. The
numbers are truly alarming. Yet these numbers mark hope for these soldiers whose performance is impacted post-injury and whose lives as veterans are impacted negatively, both at work and at home.
According to Katherine Helmick, deputy director of theDefense and Veterans Brain Injury Center in Silver Spring, Md., which was created by the government after the first Gulf War, “The natural trajectory is that you get better. It becomes more complex if you don’t get this detected early.”
Though there is a focus on the wars, 80 percent of military TBI diagnoses occurred in non-deployment settings, for instance in training. Scores of service members were never screened prior to the new policies and may be living with TBI. “I am sure the numbers are underreported,” Helmick said.
And in the civilian population
Traumatic brain injury (TBI) is a serious public health problem in the United States. Each year, traumatic brain injuries contribute to a substantial number of deaths and cases of permanent disability. Every year, at least 1.7 million TBIs occur either as an isolated injury or along with other injuries.
Brain Advanced Access (September 14, 2007), describes this phenomenon of chronic Traumatic Brain Injury in medical terms that the layperson can readily understand.
Neurobehavioural deficits, especially in cognition, are often the cause of significant disability after TBI (CDC, 2003). Observed cognitive changes that follow TBI can include decreased mental flexibility, trouble shifting sets, impaired attention, poor planning, lack of organization, problems with sequencing, impaired judgment, deficits in verbal fluency, problems with working memory, as well as increased impulsivity (Levin and Kraus, 1994; Miller, 2000; Godefroy, 2003).
So, really, that’s the point. Chronic repercussions of TBI include deficits that significantly impair everything about the routine lives of survivor.
So we know what it is… So what?
Diagnosis of TBI – getting to the bottom of it is one thing, but in the meantime, TBI sufferers are suffering.
TBI patients with or without an accurate diagnosis are still living – and will continue to live with disturbing and disruptive symptoms that affect their professional lives, their social connections, their spiritual experience, their emotional wellbeing – as well as their day to day, routine activities of daily living. We wring our hands, trying to determine if some responsible party can be persuaded to offer sufficient benefits to offset the disruption to their health and their lives. And, for certain, those who have unwittingly sacrificed their very ’selves’ – in every sense of the word – for our safety – or pleasure – deserve to be made as ‘whole’ as possible. But, of course, the fact is that you cannot place a dollar value on a person’t ability to fully experience the joys, the hardships and the routine of daily living.
Perhaps at some point in the future, diagnosis of the underlying organic pathology of TBI will lead to better understanding. Hopefully, eventually understanding will lead to treatment. And, finally, perhaps treatment will lead to reversal of the damage – and, hopefully, efforts will ultimately lead to a cure. In the meantime, however, TBI patients still have lives to lead. Mild chronic TBI inhibits short term memory and seriously impairs everyday function, which leads to problems both at work and at home. Regrettably, if the problem is sufficiently subtle TBI may not even be suspected; and the sufferer suffers even more. For those living with TBI the future can’t come soon enough.